November 20, 2014:
A recently discovered protein complex known as STING plays a crucial role in detecting the presence of tumor cells and promoting an aggressive anti-tumor response by the body's innate immune system, according to two separate studies published in the Nov. 20 issue of the journal Immunity.
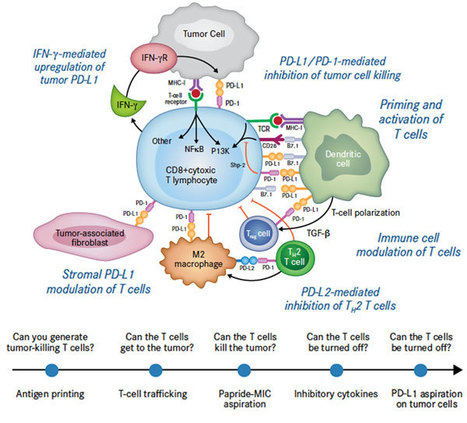
The studies, both from University of Chicago-based research teams, have major implications for the growing field of cancer immunotherapy. The findings show that when activated, the STING pathway triggers a natural immune response against the tumor. This includes production of chemical signals that help the immune system identify tumor cells and generate specific killer T cells. The research also found that targeted high-dose radiation therapy dials up the activation of this pathway, which promotes immune-mediated tumor control.
These findings could “enlarge the fraction of patients who respond to immunotherapy with prolonged control of the tumor,” according to a commentary on the papers by the University of Verona's Vincenzo Bronte, MD. “Enhancing the immunogenicity of their cancers might expand the lymphocyte repertoire that is then unleashed by interference with checkpoint blockade pathways,” such as anti-PD-1.
STING, short for STimulator of INterferon Genes complex, is a crucial part of the process the immune system relies on to detect threats -- such as infections or cancer cells -- that are marked by the presence of DNA that is damaged or in the wrong place, inside the cell but outside the nucleus.
Detection of such “cytosolic” DNA initiates a series of interactions that lead to the STING pathway. Activating the pathway triggers the production of interferon-beta, which in turn alerts the immune system to the threat, helps the system detect cancerous or infected cells, and ultimately sends activated T cells into the battle.
Via
Krishan Maggon



 Your new post is loading...
Your new post is loading...











Cancer Cell
Volume 27, Issue 4, p439–449, 13 April 2015
The Journey from Discoveries in Fundamental Immunology to Cancer ImmunotherapyJacques F.A.P. Miller, Michel Sadelain DOI: http://dx.doi.org/10.1016/j.ccell.2015.03.007