 Your new post is loading...
 Your new post is loading...
Abstract Molecular profiles of tumors and tumor-associated cells hold great promise as biomarkers of clinical outcomes. However, existing data sets are fragmented and difficult to analyze systematically. Here we present a pan-cancer resource and meta-analysis of expression signatures from ~18,000 human tumors with overall survival outcomes across 39 malignancies. By using this resource, we identified a forkhead box MI (FOXM1) regulatory network as a major predictor of adverse outcomes, and we found that expression of favorably prognostic genes, including KLRB1(encoding CD161), largely reflect tumor-associated leukocytes. By applying CIBERSORT, a computational approach for inferring leukocyte representation in bulk tumor transcriptomes, we identified complex associations between 22 distinct leukocyte subsets and cancer survival. For example, tumor-associated neutrophil and plasma cell signatures emerged as significant but opposite predictors of survival for diverse solid tumors, including breast and lung adenocarcinomas. This resource and associated analytical tools (http://precog.stanford.edu) may help delineate prognostic genes and leukocyte subsets within and across cancers, shed light on the impact of tumor heterogeneity on cancer outcomes, and facilitate the discovery of biomarkers and therapeutic targets.
Via Krishan Maggon
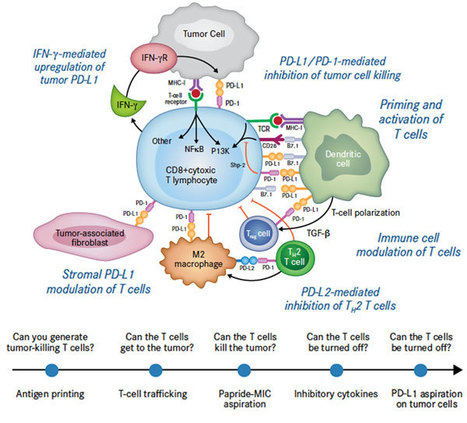
By Hanna Starobinets Staff Writer Live from the Tumor Immunology Keystone Symposium in Banff, Canada Tumors are not just solid masses of cancer cells.
Via Krishan Maggon
Abstract The immune system can remember a previously experienced pathogen and can evoke an enhanced response to reinfection that depends on memory lymphocyte populations. Recent advances in tracking antigen-experienced memory B cells have revealed the existence of distinct classes of cells that have considerable functional differences. Some of these differences seem to be determined by the stimulation history during memory cell formation. To induce rapid recall antibody responses, the contributions of other types of cells, such as memory T follicular helper cells, have also now begun to be appreciated. In this Review, we discuss these and other recent advances in our understanding of memory B cells, focusing on the underlying mechanisms that are required for rapid and effective recall antibody responses.
Via Krishan Maggon
Abstract Natural Killer (NK) cells are innate immune effectors that are primarily involved in immunosurveillance to spontaneously eliminate malignantly transformed and virally infected cells without prior sensitization. NK cells trigger targeted attack through release of cytotoxic granules, and secrete various cytokines and chemokines to promote subsequent adaptive immune responses. NK cells selectively attack target cells with diminished major histocompatibility complex (MHC) class I expression. This “Missing-self” recognition by NK cells at first puzzled researchers in the early 1990s, and the mystery was solved with the discovery of germ line encoded killer immunoglobulin receptors that recognize MHC-I molecules. This review summarizes the biology of NK cells detailing the phenotypes, receptors and functions; interactions of NK cells with dendritic cells (DCs), macrophages and T cells. Further we discuss the various strategies to modulate NK cell activity and the practice of NK cells in cancer immunotherapy employing NK cell lines, autologous, allogeneic and genetically engineered cell populations.
Via Krishan Maggon
AJMC Panel Explores Immuno-oncology, and What Making Cancer a Chronic ...
Via Krishan Maggon
Abstract Natural Killer (NK) cells use germ line encoded receptors to detect diseased host cells. Despite the invariant recognition structures, NK cells have a significant ability to adapt to their surroundings, such as the presence or absence of MHC class I molecules. It has been assumed that this adaptation occurs during NK cell development, but recent findings show that mature NK cells can also adapt to the presence or absence of MHC class I molecules. Here, we summarize how NK cells adjust to changes in the expression of MHC class I molecules. We propose an extension of existing models, in which MHC class I recognition during NK cell development sequentially instructs and maintains NK cell function. The elucidation of the molecular basis of the two effects may identify ways to improve the fitness of NK cells and to prevent the loss of NK cell function due to persistent alterations in their environment..
Via Krishan Maggon
|
Clinical & Translational Immunology Abstract A novel conception of CD4+ T cells with cytolytic potential (CD4+ CTL) is emerging. These cells appear to have a part in controlling malignancies and chronic infections. Human parvovirus B19 can cause a persistent infection, yet no data exist on the presence of B19-specific CD4+ CTLs. Such cells could have a role in the pathogenesis of some autoimmune disorders reported to be associated with B19. We explored the cytolytic potential of human parvovirus B19-specific T cells by stimulating peripheral blood mononuclear cell (PBMC) with recombinant B19-VP2 virus-like particles. The cytolytic potential was determined by enzyme immunoassay-based quantitation of granzyme B (GrB) and perforin from the tissue culture supernatants, by intracellular cytokine staining (ICS) and by detecting direct cytotoxicity. GrB and perforin responses with the B19 antigen were readily detectable in B19-seropositive individuals. T-cell depletion, HLA blocking and ICS experiments showed GrB and perforin to be secreted by CD4+ T cells. CD4+ T cells with strong GrB responses were found to exhibit direct cytotoxicity. As anticipated, ICS of B19-specific CD4+ T cells showed expected co-expression of GrB, perforin and interferon gamma (IFN-γ). Unexpectedly, also a strong co-expression of GrB and interleukin 17 (IL-17) was detected. These cells expressed natural killer (NK) cell surface marker CD56, together with the CD4 surface marker. To our knowledge, this is the first report on virus-specific CD4+ CTLs co-expressing CD56 antigen. Our results suggest a role for CD4+ CTL in B19 immunity. Such cells could function within both immune regulation and triggering of autoimmune phenomena such as systemic lupus erythematosus (SLE) or rheumatoid arthritis.
Via Krishan Maggon
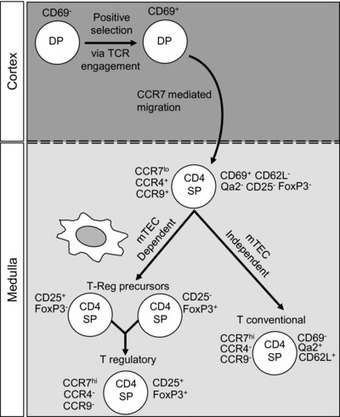
Abstract The organization of the thymus into distinct cortical and medullary regions enables it to control the step-wise migration and development of immature T-cell precursors. Such a process provides access to specialized cortical and medullary thymic epithelial cells at defined stages of maturation, ensuring the generation of self-tolerant and MHC-restricted conventional CD4+ and CD8+ αβ T cells. The migratory cues and stromal cell requirements that regulate the development of conventional αβ T cells have been well studied. However, the thymus also fosters the generation of several immunoregulatory T-cell populations that form key components of both innate and adaptive immune responses. These include Foxp3+ natural regulatory T cells, invariant γδ T cells, and CD1d-restricted invariant natural killer T cells (iNKT cells). While less is known about the intrathymic requirements of these nonconventional T cells, recent studies have highlighted the importance of the thymus medulla in their development. Here, we review recent findings on the mechanisms controlling the intrathymic migration of distinct T-cell subsets, and relate this to knowledge of the microenvironmental requirements of these cells.
Via Krishan Maggon
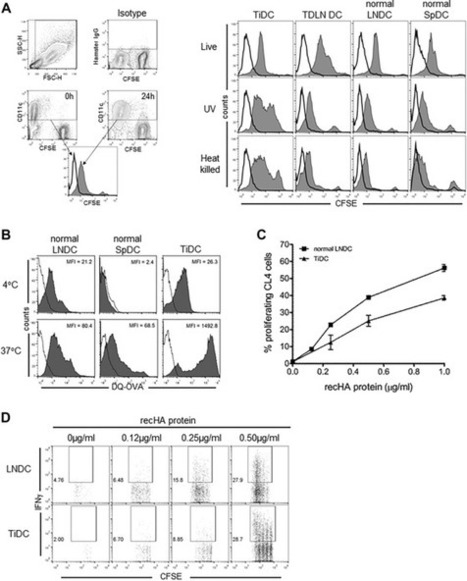
Abstract Cross-presentation defines the unique capacity of an APC to present exogenous Ag via MHC class I molecules to CD8+ T cells. DCs are specialized cross-presenting cells and as such have a critical role in antitumor immunity. DCs are routinely found within the tumor microenvironment, but their capacity for endogenous or therapeutically enhanced cross-presentation is not well characterized. In this study, we examined the tumor and lymph node DC cross-presentation of a nominal marker tumor Ag, HA, expressed by the murine mesothelioma tumor AB1-HA. We found that tumors were infiltrated by predominantly CD11b+ DCs with a semimature phenotype that could not cross-present tumor Ag, and therefore, were unable to induce tumor-specific T-cell activation or proliferation. Although tumor-infiltrating DCs were able to take up, process, and cross-present exogenous cell-bound and soluble Ags, this was significantly impaired relative to lymph node DCs. Importantly, however, systemic chemotherapy using gemcitabine reversed the defect in Ag cross-presentation of tumor DCs. These data demonstrate that DC cross-presentation within the tumor microenvironment is defective, but can be reversed by chemotherapy. These results have important implications for anticancer therapy, particularly regarding the use of immunotherapy in conjunction with cytotoxic chemotherapy.
Via Krishan Maggon
Abstracts from the ESMO Symposium on Immuno-Oncology 2014 are now available
Via Krishan Maggon
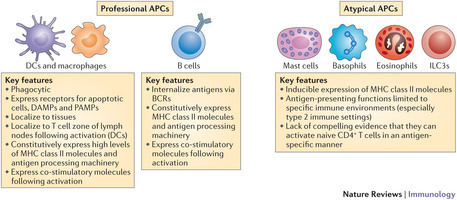
Dendritic cells, macrophages and B cells are regarded as the classical antigen-presenting cells of the immune system. However, in recent years, there has been a rapid increase in the number of cell types that are suggested to present antigens on MHC class II molecules to CD4+ T cells. In this Review, we describe the key characteristics that define an antigen-presenting cell by examining the functions of dendritic cells. We then examine the functions of the haematopoietic cells and non-haematopoietic cells that can express MHC class II molecules and that have been suggested to represent 'atypical' antigen-presenting cells. We consider whether any of these cell populations can prime naive CD4+ T cells and, if not, question the effects that they do have on the development of immune responses.
Via Krishan Maggon
Lung cancer uses cunning mechanisms to evade the immune system. Can new antibody therapies outwit the disease?
Via Krishan Maggon
|



 Your new post is loading...
Your new post is loading...
















NATURE MEDICINE | RESOURCE
The prognostic landscape of genes and infiltrating immune cells across human cancersAndrew J Gentles,Aaron M Newman,Chih Long Liu,Scott V Bratman,Weiguo Feng,Dongkyoon Kim,Viswam S Nair,Yue Xu,Amanda Khuong,Chuong D Hoang,Maximilian Diehn,Robert B West,Sylvia K Plevritis& Ash A AlizadehAffiliationsContributionsCorresponding authorNature Medicine (2015) doi:10.1038/nm.3909Received 19 January 2015 Accepted 19 June 2015 Published online 20 July 2015